H2Know
Class Summary
BioDesign is a graduate class centered around medical device design. We learned about not only market fit, research, and ideation processes, but also the business side of products, such as creating business plans and pro formas. For our final project, we applied those lessons to the problem of chronic dehydration in hospital patients. We developed an integrated sensor system to actively monitor patient fluid balance to reduce caregiver cognitive load to improve patient health.
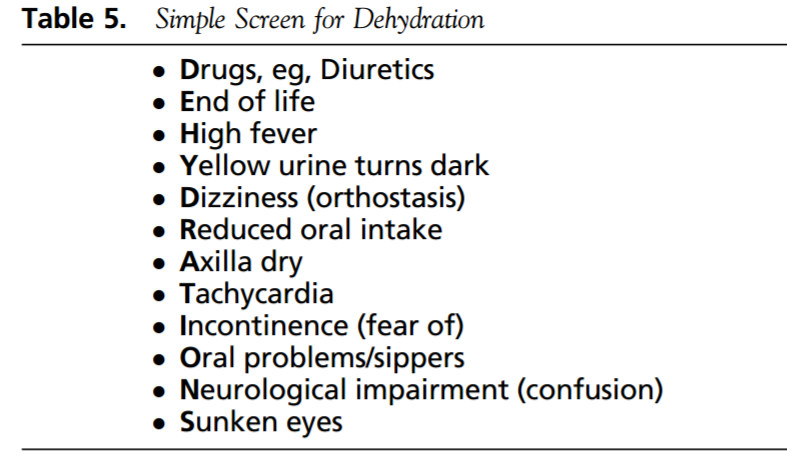
There are 13 ways to identify dehydration, which can be conveniently and quickly remembered with the acronym DEHYDRATIONS.
Background
Post admission dehydration (PAD) can be difficult to detect since no single sign is indicative of dehydration. Despite the lack of testing available, PAD can have dire consequences for patients such as increased mortality risk and decreased quality of life. In severe cases, it can lead to mental issues and death.
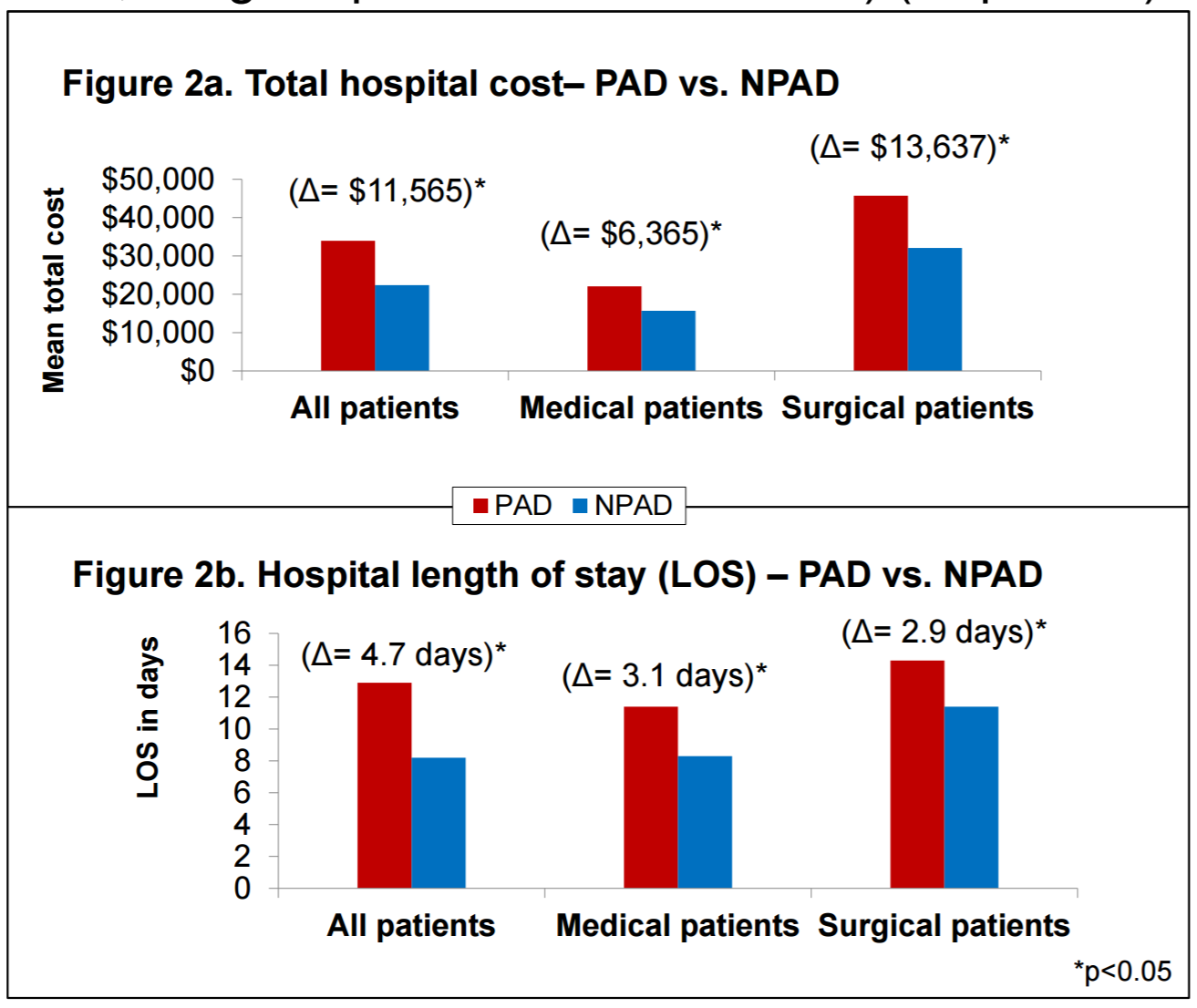
For hospitals, increased readmission rates and slower healing rates means more money spent on a patient. There’s avoidable costs due to excessive treatment, ranging from $11,000 to 13,000 per patient. Patients with PAD can stay 2.9 – 4.7 days longer than needed, tallying up to 1.14 billion spent on preventable hospitalizations.
Our addressable market comes from the 900,000 hospital beds distributed among the nation’s 5,500 hospitals. We focused initially on people over the age of 65 as they are more susceptible to dehydration. We found that 20 million people over 65 admitted to the emergency department annually, with 6 million of them continuing on to be admitted to the hospital.
Process
After looking at clinical need from a research basis, we chose to focus on patients in a closely monitored setting, specifically those over 65 in a hospital setting that were not in the intensive care unit. We found that patients have trouble staying hydrated for a variety of reasons and they are difficult to track, especially in the elderly, who are a vulnerable population.
IVs were ruled out since breaking the skin barrier increases infection. We also knew our product would have to be hygienic - single-use products can be sterilized, but can incur higher costs.
Initially, we focused on patients who were too weak to lift the water jug and examined ways to dispense water, such as through stabilized cups or bottom-fill cups. We concluded that an easier-to-lift jug was too much of a gradual improvement to be valuable.
Weighing the cups and jugs was an option that we explored, but this offset the work on caregivers. The system was too fragile since it wouldn’t account for IV fluids or unsanctioned refills or spills.
I had to opportunity to shadow in an intensive care unit and learned more about how healthcare providers use data. As such, we started thinking about tracking water instead. We wanted to provide data without having someone manually transcribe, since this would drastically increase error rates. Concurrently, I began reading about holistic approaches to hydration and thinking of consuming water as a preventative measure. From there, we continued to think of water as medicine.
This holistic school of thinking encourages personalization and patient input. We wanted to incentivize water consumption through personalization. Our first attempt was a build-your-own menu approach to water temperature and other variables. However, this would be a one-per-patient procedure change that could be incorporated into whatever we created.
Product
Our final needs statement: Improve hydration management for the assisted living population through preventative approaches. Our executive summary explains some of these points in more detail.
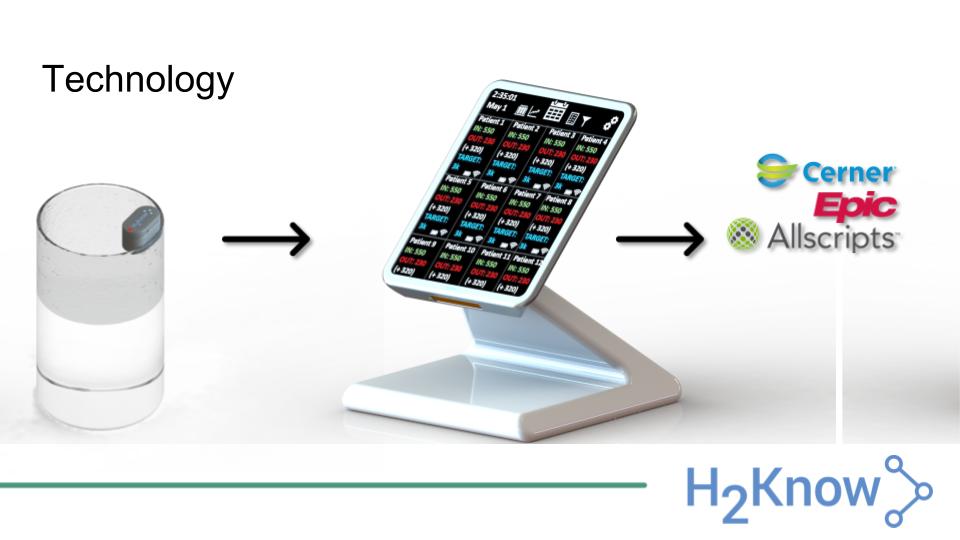
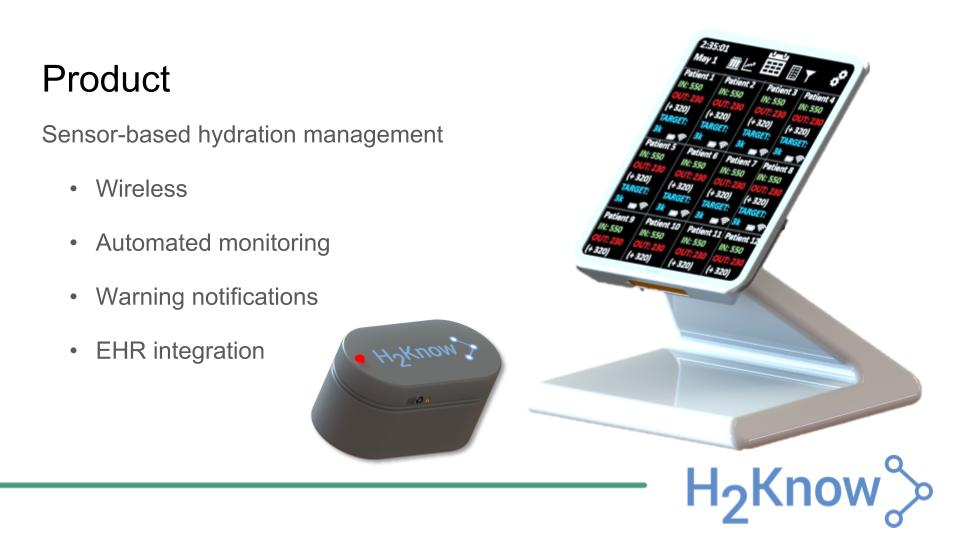
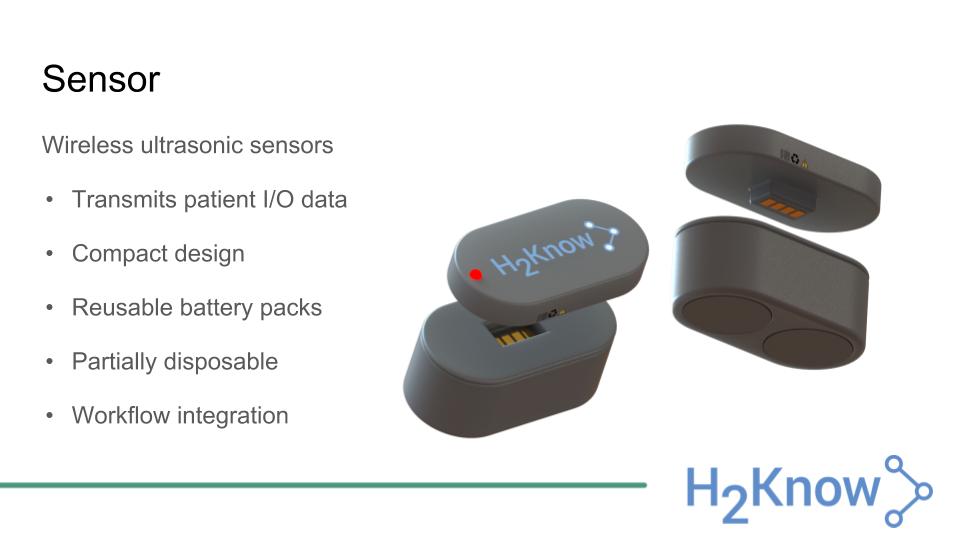
We developed a sensor-based hydration management that would integrate with the Electronic Health Record (EHR). It consists of a wireless ultrasdonic sensor and a receiver station.
The method allows for variety in water consumption without being obtrusive. By eliminating the need for manual entry of input and outputs, it decreases workload to caregiver and gives easy access to quantifiable data with meaningful use. By introducing standardization and the visibility of hydration, the system decreases the prevalence of PAD, length of stay, and rates of readmission. We approached this from a cost reduction standpoint and hope that it will lead to an increase in patient clinical outcomes.
Business Plan
We would pursue a licensing strategy where we would partner with a medical goods manufacturer for: Distribution channels and supply chain management, large-scale manufacturing, integration with currently-used products, and marketing assistance.
Our five-year plan:
- Further develop the technology
- FDA submission (Class I 510(k) ) and plan clinical efficacy studies
- Low-volume manufacturing for Clinical efficacy study & marketing strategy
- Licensing partner, begin development of sensor V2
- Expand scope of application and develop next product
Future Work
Manufacturing and implementing the sensors and system would require the cooperation of hospitals. In addition, we struggled with the classification of our system under insurance codes. After our pitch, we were approached by an investor from the Cleveland Clinic but ultimately did not move forward with commercializing the product.